Be cautious with azithromycin, especially if you’re dealing with underlying auditory issues. Research indicates a potential link between this antibiotic and ototoxicity, particularly within specific patient groups. Monitoring hearing function during treatment may protect against progressive hearing loss.
Multiple studies have explored azithromycin’s impact on auditory health. Some findings reveal a risk of transient hearing disturbances, particularly in patients receiving high doses for extended periods. It’s important to balance the benefits of treating infections with the risks associated with hearing loss. Ensure clinicians are aware of a patient’s medical history, especially concerning hearing problems.
Consider alternative treatments if the risk is deemed significant. Patients with renal impairment, for example, may require adjusted dosages or close observation. Regular audiometric evaluations provide a proactive approach to detect any changes in hearing early, allowing for timely interventions. Building a comprehensive treatment plan that includes these considerations can significantly enhance patient outcomes.
- Azithromycin and Ototoxicity: Understanding the Risks
- Identifying Symptoms
- Best Practices in Prescribing
- Mechanism of Action: How Azithromycin Works
- Historical Context of Ototoxicity in Antibiotic Treatment
- Understanding Ototoxic Mechanisms
- Current Recommendations and Monitoring Strategies
- Evidence Linking Azithromycin to Ototoxic Effects
- Patient Populations at Higher Risk for Ototoxicity
- Symptoms and Signs of Ototoxicity After Azithromycin Use
- Preventive Measures for Azithromycin-Induced Ototoxicity
- Regular Auditory Assessments
- Patient Education
- Alternatives to Azithromycin in Suspected Ototoxic Cases
Azithromycin and Ototoxicity: Understanding the Risks
Monitor patients closely for signs of ototoxicity when prescribing azithromycin. This antibiotic, commonly used to treat various infections, has been associated with auditory side effects in certain populations, particularly those with pre-existing conditions affecting hearing. Research indicates that the risk of ototoxicity increases in individuals who are on prolonged treatment regimens or those receiving high doses.
Identifying Symptoms
Be vigilant for symptoms such as tinnitus, hearing loss, or balance issues. Patients should report any auditory changes immediately, allowing for timely intervention. Regular audiological assessments may be advisable for patients at higher risk, including those with renal impairment or concurrent use of other ototoxic medications.
Best Practices in Prescribing
Use the lowest effective dose of azithromycin for the shortest duration necessary to minimize risk. Review patient history to identify other factors that could compound the likelihood of ototoxic effects. Educating patients about potential side effects empowers them to seek help promptly if they experience changes in their hearing. By staying informed and proactive, healthcare providers can mitigate the risks associated with azithromycin use.
Mechanism of Action: How Azithromycin Works
Azithromycin targets bacterial protein synthesis through binding to the 50S subunit of the ribosome. This binding inhibits the translocation step of protein synthesis, effectively stopping the growth of bacteria. By interfering with the translation of proteins, azithromycin prevents bacteria from replicating and spreading.
This antibiotic exhibits a broad spectrum of activity, which includes common pathogens such as Streptococcus pneumoniae and Haemophilus influenzae. In addition to its antibacterial action, azithromycin also possesses anti-inflammatory properties, making it particularly useful in respiratory infections.
Azithromycin’s long half-life allows for once-daily dosing, enhancing patient compliance. It accumulates in tissues, especially in the lungs, providing sustained therapeutic levels that help in combating infection even after the medication course is completed.
Pharmacokinetics play a key role in its effectiveness. Azithromycin achieves high concentrations in inflammatory cells and tissues, assisting in clearing infections more efficiently. This characteristic contributes to its use in treating chronic inflammatory conditions, such as asthma.
Understanding azithromycin’s mechanism aids in maximizing its clinical applications while minimizing the risk of side effects, like ototoxicity. Monitoring auditory function in patients taking high doses or prolonged therapy is advisable to prevent potential damage.
Historical Context of Ototoxicity in Antibiotic Treatment
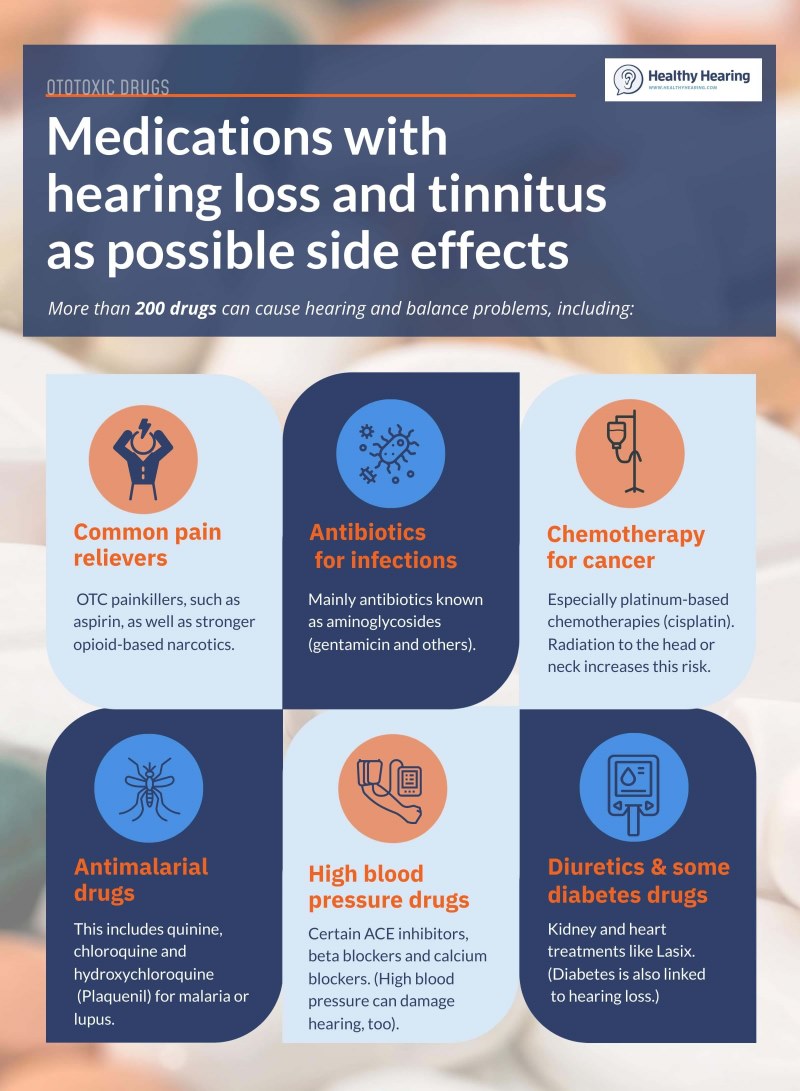
Antibiotics have revolutionized medical treatment but have also revealed risks, such as ototoxicity. In the early 20th century, the introduction of sulfonamides marked significant progress; however, adverse effects remained underexplored. The emergence of aminoglycosides in the 1940s raised alarms as they presented a higher risk of hearing loss and balance disorders.
The pivotal moment came in the 1970s with studies linking streptomycin and other aminoglycosides to permanent auditory damage. Researchers began to recognize that ototoxicity could result from dosage, duration of treatment, and individual patient susceptibility. This prompted further investigation into safer antibiotic alternatives, leading to the advent of macrolides, such as azithromycin.
Understanding Ototoxic Mechanisms
Modern research identifies specific pathways through which certain antibiotics induce ototoxic effects. Direct damage to the inner ear structures, inflammation, and oxidative stress are key factors. This understanding helps clinicians anticipate risks associated with antibiotic prescriptions and implement monitoring strategies for at-risk populations.
Current Recommendations and Monitoring Strategies
Healthcare providers now advocate for cautious prescribing practices. Regular hearing assessments and patient education about recognizing early signs of hearing impairment are imperative. Utilizing alternative antibiotics with a lower risk profile, such as azithromycin, is recommended when appropriate. Maintaining a strong communication line with patients regarding potential side effects can significantly enhance treatment outcomes.
| Antibiotic Class | Ototoxic Risk |
|---|---|
| Aminoglycosides | High |
| Macrolides (e.g., Azithromycin) | Low |
| Vancomycin | Moderate |
Today’s antibiotic treatment continues to evolve, embracing safer options while acknowledging past experiences with ototoxicity. Awareness and research remain essential in guiding clinical practices to mitigate risks effectively.
Evidence Linking Azithromycin to Ototoxic Effects
Recent studies indicate a potential connection between azithromycin use and ototoxicity. Clinical observations highlight instances where patients developed hearing loss following azithromycin treatment, particularly those with pre-existing kidney issues or concurrent use of other ototoxic medications. A meta-analysis of data revealed that a small percentage of patients experienced auditory disturbances, reinforcing these observations.
Research indicates that azithromycin could disrupt cellular mechanisms in the cochlea. Specifically, it may affect mitochondrial function and lead to oxidative stress, contributing to hair cell damage in the inner ear. This mechanism appears particularly impactful for high doses or prolonged treatments.
Healthcare providers should apply caution when prescribing azithromycin, particularly for vulnerable populations, such as the elderly or those with hearing impairments. Regular monitoring of auditory function in at-risk patients during azithromycin therapy may prove beneficial. Early detection of ototoxicity allows for timely intervention and better patient outcomes.
In conclusion, while azithromycin remains a critical antibiotic, acknowledgement of its potential ototoxic effects is necessary. Continued research and vigilant patient management will help mitigate associated risks and enhance treatment efficacy.
Patient Populations at Higher Risk for Ototoxicity
Individuals who take azithromycin should be aware of specific patient populations that face a heightened risk of ototoxicity. These groups require careful monitoring and, if possible, alternative treatment options.
- Older Adults: Age-related changes in auditory function make older individuals more sensitive to ototoxic effects.
- Patients with Pre-existing Hearing Loss: Those who already have hearing impairments are more likely to experience exacerbated symptoms.
- Individuals on Concurrent Ototoxic Medications: Combining azithromycin with other ototoxic drugs, such as certain chemotherapy agents or high doses of loop diuretics, increases risk.
- Patients with Renal Impairment: Reduced kidney function can lead to higher systemic concentrations of azithromycin, raising the likelihood of adverse effects, including ototoxicity.
- Children: Pediatric patients can exhibit different susceptibilities to drug effects, necessitating extra caution when prescribing azithromycin.
Healthcare providers should evaluate these risk factors before prescribing azithromycin. Close audiological monitoring may be warranted, particularly for patients in the aforementioned groups. Seeking alternatives and adjusting dosages can mitigate risks while ensuring effective treatment.
Symptoms and Signs of Ototoxicity After Azithromycin Use
Monitor for changes in hearing after taking azithromycin. Common symptoms include tinnitus, which manifests as ringing or buzzing in the ears. Patients may also report muffled hearing or sudden loss of hearing in one or both ears.
Another sign to look for is imbalance or dizziness, often associated with ear function. Individuals might experience a feeling of unsteadiness when standing or walking. Pay attention to any unusual difficulties with spatial orientation.
Evaluate the onset and duration of these symptoms. Ototoxic effects can appear shortly after beginning treatment or even after completing a course of azithromycin. Document any correlations between new symptoms and medication use.
Consider conducting a hearing assessment if symptoms develop. Audiometric tests can help determine the extent of hearing impairment and differentiate between conductive and sensorineural hearing loss.
If ototoxicity is suspected, consult a healthcare professional for further evaluation and management. Adjusting medication or considering alternatives may be necessary to mitigate symptoms and preserve hearing function.
Preventive Measures for Azithromycin-Induced Ototoxicity
Monitor the dosage closely. Prescribe the lowest effective dose for the shortest duration necessary. This approach minimizes risks associated with ototoxicity.
Regular Auditory Assessments
- Conduct baseline hearing tests prior to starting treatment.
- Schedule follow-up audiometric evaluations throughout and after the course of azithromycin.
- Pay attention to any reported changes in hearing or balance.
Patient Education
- Inform patients about potential ototoxic effects.
- Encourage reporting of symptoms like tinnitus, dizziness, or hearing loss immediately.
- Discuss alternatives if patients have a history of ototoxicity with other medications.
Consider potential drug interactions. Review the patient’s entire medication regimen to eliminate or reduce the risk of concurrent ototoxic agents.
Re-evaluate the necessity of azithromycin. Explore alternative antibiotics when appropriate based on specific infections.
Maintain hydration. Encourage patients to stay well-hydrated to support the kidneys and overall medication clearance.
Alternatives to Azithromycin in Suspected Ototoxic Cases
Consider using doxycycline or amoxicillin as substitutes for azithromycin in cases where ototoxicity is a concern. Doxycycline, a tetracycline antibiotic, effectively treats a variety of bacterial infections without the associated risks of ototoxicity. It is often used in respiratory tract infections and offers a favorable safety profile.
Amoxicillin, a penicillin derivative, is another viable option that can address many common infections. It is particularly useful for respiratory and ear infections, presenting a lower risk for auditory complications compared to macrolides like azithromycin.
Clindamycin serves as an alternative for patients allergic to penicillins or tetracyclines. It targets anaerobic bacteria and can be effective in treating severe skin infections, soft tissue infections, and some respiratory infections. Monitoring renal function is advisable as it has potential side effects related to the kidneys.
For patients with suspected mycoplasma infections, consider using fluoroquinolones, such as levofloxacin. This class of antibiotics is effective against various pathogens and has a reduced risk of ototoxicity. Always assess the risk-benefit ratio, especially for those with pre-existing risk factors for hearing damage.
Consult with an infectious disease specialist to evaluate the best course of action tailored to individual patient circumstances. This collaboration ensures the choice of appropriate antibiotics while minimizing the risk of ototoxicity and maintaining effective infection control.