Monitor azithromycin resistance rates closely to adapt your treatment plans for bacterial infections effectively. Recent studies indicate that resistance rates can vary significantly across different regions, highlighting the necessity for local data to inform antibiotic use.
In the United States, azithromycin resistance among common pathogens, such as Streptococcus pneumoniae and Haemophilus influenzae, has been observed at rates around 15% to 30%. These figures underscore the importance of susceptibility testing before prescribing azithromycin.
Internationally, the situation displays alarming variation. For instance, in parts of Southeast Asia, reports show resistance rates exceeding 50%. This geographic disparity makes it crucial for healthcare providers to stay informed about local antibiograms to ensure the selection of appropriate antibiotics.
Consider alternative regimens or combination therapies when resistance is apparent. Utilizing a targeted approach tailored to local resistance patterns will enhance patient outcomes and help combat the growing threat of antibiotic resistance.
- Azithromycin Resistance Rates
- Factors Influencing Resistance
- Strategies to Combat Resistance
- Overview of Azithromycin
- Indications for Use
- Resistance Concerns
- Global Trends in Azithromycin Resistance
- Regional Resistance Patterns
- Impact on Treatment Outcomes
- Geographic Variability in Resistance Rates
- Factors Contributing to Resistance
- Impact of Azithromycin Resistance on Public Health
- Clinical Implications for Treatment
- Strategies to Combat Azithromycin Resistance
- Future Directions in Research and Monitoring
Azithromycin Resistance Rates
Healthcare professionals should closely monitor azithromycin resistance rates, particularly among common pathogens such as Streptococcus pneumoniae and Neisseria gonorrhoeae. Current data indicates that resistance in S. pneumoniae has reached approximately 30% in some regions, significantly impacting treatment outcomes. Regular susceptibility testing remains critical to guide appropriate therapy.
Factors Influencing Resistance
Several factors contribute to the rise in azithromycin resistance. Over-prescription of the antibiotic, especially in outpatient settings, plays a significant role. Misdiagnosis of viral infections leads to unnecessary usage, enhancing selective pressure on bacterial populations. Additionally, global travel and antibiotic usage patterns in various countries create disparities in resistance rates.
Strategies to Combat Resistance
Implementing stewardship programs can effectively reduce resistance rates. Educating healthcare providers on guidelines will ensure azithromycin is prescribed only when indicated. Patient awareness campaigns can also help reduce expectations for antibiotics when they are not needed. Regular surveillance of resistance patterns will support informed decision-making and optimize treatment protocols.
Overview of Azithromycin
Azithromycin is a macrolide antibiotic with broad-spectrum activity against various bacteria. It effectively treats respiratory tract infections, skin infections, and sexually transmitted diseases. The drug inhibits bacterial protein synthesis by binding to the 50S ribosomal subunit, preventing the growth and reproduction of bacteria.
Indications for Use
Common indications for azithromycin include:
- Pneumonia
- Bronchitis
- Sinusitis
- Chlamydia infections
- Skin and soft tissue infections
The drug is often prescribed as a single dose for certain infections, like chlamydia, making treatment more convenient for patients.
Resistance Concerns
Resistance rates to azithromycin have been increasing in several bacterial strains, particularly in Streptococcus pneumoniae and Neisseria gonorrhoeae. Monitoring resistance patterns is critical for effective treatment. Healthcare providers should consider local resistance data when prescribing azithromycin. Alternative antibiotics may be necessary for infections in areas with high resistance rates.
Using azithromycin judiciously can help preserve its effectiveness. Following appropriate prescribing guidelines and patient adherence to treatment regimens are essential steps in combating resistance.
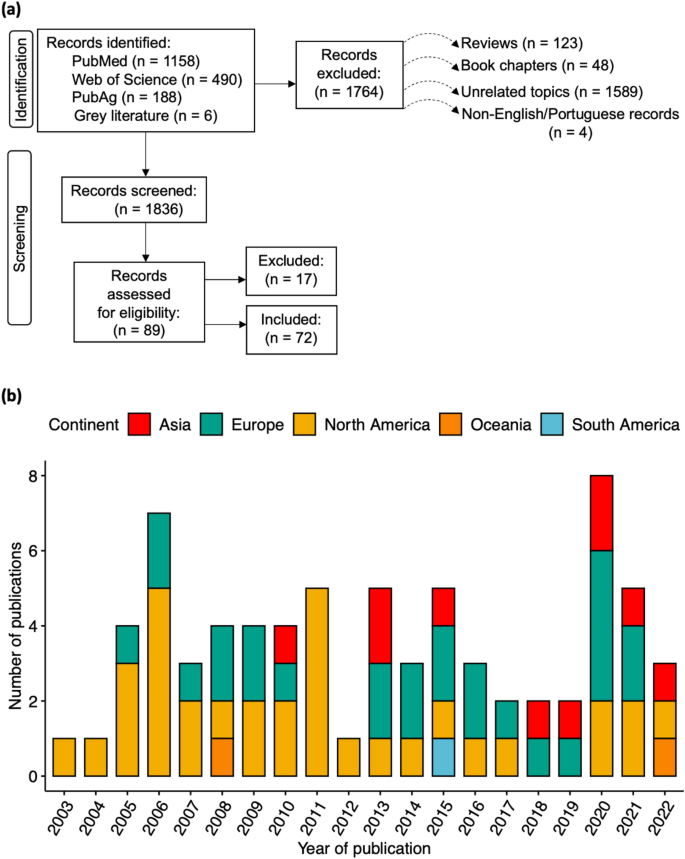
Global Trends in Azithromycin Resistance
Addressing azithromycin resistance is a priority in public health globally. Data indicates that resistance rates have considerably increased in various regions. For instance, countries in East Africa report resistance rates exceeding 40%, while regions in South America and Southeast Asia show similar patterns.
Regional Resistance Patterns
In Europe, azithromycin resistance varies, with Mediterranean countries experiencing higher rates, often due to increased macrolide prescriptions. Conversely, Northern European countries maintain lower resistance levels. Surveillance programs must adapt to these trends to inform local antibiotic stewardship strategies.
Impact on Treatment Outcomes
The rise in azithromycin resistance has significant implications for treatment protocols. Increasing failure rates in bacterial infections necessitate alternative therapies. Identification of resistant strains through targeted testing can guide clinical decisions and reduce the misuse of antibiotics.
| Region | Resistance Rate (%) | Primary Bacteria |
|---|---|---|
| East Africa | 45 | Neisseria gonorrhoeae |
| South America | 38 | Streptococcus pneumoniae |
| South East Asia | 42 | Haemophilus influenzae |
| Europe (Mediterranean) | 35 | Staphylococcus aureus |
| North Europe | 15 | Streptococcus pyogenes |
Continuous monitoring of resistance trends is vital for adapting treatment guidelines and policies. Public health initiatives focusing on antibiotic stewardship must prioritize reducing unnecessary prescriptions of azithromycin to mitigate resistance development.
Geographic Variability in Resistance Rates
Resistance rates to azithromycin vary significantly across different regions. In North America, studies show a resistance rate up to 25% in certain populations, particularly among young adults. This trend is influenced by the widespread use of macrolides in both therapeutic and agricultural settings.
In contrast, European countries like Sweden report much lower resistance rates, around 5%, attributed to stricter antibiotic stewardship programs and regulations. Countries such as Italy, however, experience rates closer to 20%, highlighting regional differences in prescribing practices.
In Asia, the situation presents a mixed picture. In Japan, the resistance rate is approximately 15%, while in parts of India, studies reveal rates climbing to 35% due to indiscriminate use of antibiotics. Surveillance reports emphasize the need for local guidelines to tailor prevention strategies effectively.
Healthcare providers should be aware of these geographic patterns when considering azithromycin for treatment. Regular susceptibility testing can provide critical insights and help inform appropriate antibiotic use in various settings. Collaboration between healthcare facilities and public health organizations remains crucial to monitor and combat resistance trends effectively.
Investing in continued education on antibiotic resistance and implementing local policies can further combat the rise of resistance rates. Addressing this issue through community awareness and responsible prescribing habits will contribute to better patient outcomes and public health. Regularly updated data on local resistance patterns can serve as a valuable resource for clinicians.
Factors Contributing to Resistance
Inadequate dosing and incomplete treatment courses significantly elevate the risk of azithromycin resistance. Ensuring proper dosage and adherence to the full treatment regimen prevents the survival of resistant bacteria. Clinicians should educate patients about the importance of completing their prescribed antibiotics.
Overuse and misuse of antibiotics in both human and veterinary medicine contribute to resistance. Limiting azithromycin prescriptions to necessary cases, such as confirmed bacterial infections, helps diminish resistance rates. Healthcare providers must evaluate the need for azithromycin carefully and consider alternative treatments when appropriate.
Environmental factors, such as antibiotic contamination in water sources, can also promote resistance. Regular monitoring and stricter regulations on waste disposal in pharmaceutical manufacturing are vital. Initiatives to reduce antibiotic runoff into ecosystems can safeguard public health and combat the spread of resistant strains.
Cross-resistance is another concerning element. Bacteria exposed to various antibiotics can develop mechanisms that confer resistance to azithromycin as well. Utilizing combination therapies may reduce the risk of such cross-resistance, enhancing the effectiveness of treatment strategies.
Education on proper antibiotic use among healthcare professionals and the public is crucial. Continuous training sessions, workshops, and information campaigns can heighten awareness regarding the consequences of resistance. Community engagement plays an important role in spreading knowledge about responsible antibiotic usage.
Genetic factors in bacteria also influence resistance patterns. Regular genetic surveillance allows for the identification of emerging resistant strains. Research into the genetic mechanisms underlying resistance can guide the development of new treatments and strategies to address this growing concern.
Impact of Azithromycin Resistance on Public Health
Addressing azithromycin resistance requires immediate public health strategies to mitigate its effects. Increased resistance rates lead to treatment failures in bacterial infections, particularly respiratory and sexually transmitted diseases. This complicates the management of common conditions and elevates the risk of widespread outbreaks.
Studies show that azithromycin resistance has surged, with rates exceeding 30% in certain populations. This trend directly influences therapeutic options, often necessitating more potent antibiotics with higher side effects and costs. Public health initiatives must prioritize monitoring resistance patterns and educating healthcare providers on alternative treatments.
Infection control measures also need reinforcement. Hospitals should implement rigorous screening protocols and isolate cases of resistant infections promptly. Vaccination programs can reduce the incidence of infections treated with azithromycin, cutting down on the opportunities for resistance development.
Community awareness campaigns play a crucial role in this battle. Educating the public on the responsible use of antibiotics can foster better compliance with treatment guidelines and lower the demand for unnecessary prescriptions. Such initiatives help preserve the effectiveness of existing antibiotics and combat resistance trends.
Finally, integrating research efforts into public health policies ensures ongoing evaluation of resistance rates and development of new treatment guidelines. Collaborative efforts between health authorities, healthcare professionals, and researchers can lead to innovative solutions that keep azithromycin effective against resistant strains.
Clinical Implications for Treatment
Begin treatment with susceptibility testing to determine the effectiveness of azithromycin against specific pathogens. If resistance is suspected or confirmed, consider alternatives like amoxicillin or doxycycline based on the infection type.
- Bacterial Infections: For respiratory tract infections, use a combination of antibiotics if resistance is present. Macrolides can be less effective; alternatives like respiratory fluoroquinolones may provide better outcomes.
- STIs: For chlamydia, maintain azithromycin as a first-line option but confirm local resistance patterns. If high rates are reported, shift to doxycycline.
- Skin Infections: In cases of skin and soft tissue infections, evaluate cultures carefully. If resistance is prevalent, consider options such as trimethoprim-sulfamethoxazole.
Monitor treatment efficacy closely, adjusting based on clinical responses and follow-up cultures. Educate patients about the potential for resistance and the importance of completing prescribed courses.
- Implement stringent antibiotic stewardship programs to minimize inappropriate use of azithromycin.
- Encourage vaccination for preventable diseases, reducing the need for antibiotics.
- Engage in local and national surveillance programs to track resistance patterns regularly.
Staying updated on resistance trends will enhance decision-making in treatment plans. Prioritize collaboration with microbiologists for tailored therapeutic options.
Strategies to Combat Azithromycin Resistance
Implement targeted stewardship programs to monitor azithromycin use in healthcare settings. Analyze prescribing patterns regularly to identify inappropriate use and provide feedback to prescribers.
- Educate Healthcare Providers: Conduct workshops and training sessions focusing on the appropriate use of azithromycin and the implications of resistance.
- Surveillance Programs: Establish robust surveillance systems to track resistance rates in different regions and populations. Use this data to inform treatment guidelines.
- Promote Alternative Therapies: Encourage the use of alternative antibiotics when suitable, as well as combination therapies to reduce reliance on azithromycin.
Enhance public awareness about the consequences of antibiotic misuse. Inform patients about the importance of taking antibiotics only when prescribed and following instructions correctly.
- Implement Restrictions: Limit azithromycin prescriptions for non-bacterial infections through regulatory measures.
- Clinical Trials: Invest in research for new antibiotics and therapies to ensure options remain available as resistance develops.
- Infection Control Practices: Strengthen infection control measures in healthcare facilities to prevent the spread of resistant strains.
Support the development of diagnostic tools for rapid identification of bacterial infections to promote more targeted antibiotic use. This helps ensure that azithromycin is prescribed only when truly needed.
- Community Engagement: Foster partnerships with community organizations to raise awareness about antibiotic resistance.
- Veterinary Practices: Enforce appropriate use of azithromycin in veterinary medicine, as animal use contributes to resistance in humans.
Regularly update treatment guidelines based on current resistance patterns and emerging research. Engage clinicians in discussions about best practices for managing infections effectively while minimizing resistance development.
Future Directions in Research and Monitoring
Focus on implementing robust national surveillance systems to track azithromycin resistance rates across diverse geographical regions. This initiative requires collaboration between healthcare institutions, public health agencies, and research organizations to build a comprehensive database. Regular updates and accessible sharing of data will facilitate timely responses to emerging resistance patterns.
Expand research efforts to understand the mechanisms behind azithromycin resistance. Investigating genetic mutations and the role of efflux pumps can provide insights into how resistance develops and spreads. Such studies enable targeted interventions and the development of novel therapeutic strategies.
Incorporate advanced genomic and molecular techniques in resistance monitoring. Techniques like whole-genome sequencing can detect minor resistant strains, enhancing our understanding of the resistance landscape. These methods also identify potential transmission pathways and epidemiological trends, guiding public health interventions.
Encourage interdisciplinary research by integrating microbiology, pharmacology, and epidemiology. This collaboration can foster innovative approaches, such as combining azithromycin with adjuvants to counteract resistance mechanisms. Engaging experts from various fields can enhance problem-solving strategies and lead to effective alternatives.
Incorporate patient and provider education to raise awareness about antibiotic resistance. Workshops and informational campaigns can help minimize unnecessary prescriptions and promote responsible use of azithromycin. Engaging healthcare professionals in training sessions will ensure awareness of the latest resistance data and guidelines.
Invest in alternative treatments and drug development. Exploring new antibiotics or treatment regimens that can work alongside existing medications may provide solutions to resistance challenges. Clinical trials assessing the efficacy of these alternatives will be crucial in determining their viability.
| Research Focus | Action Items |
|---|---|
| National Surveillance | Establish collaborative databases and standardized reporting systems. |
| Resistance Mechanisms | Investigate genetic mutations and efflux pump roles. |
| Advanced Monitoring Techniques | Employ whole-genome sequencing to track minor resistant strains. |
| Interdisciplinary Approaches | Facilitate partnerships between microbiologists, pharmacologists, and epidemiologists. |
| Education Initiatives | Conduct training for healthcare providers on resistance management. |
| Alternative Treatments | Support clinical trials of new antibiotics and combination therapies. |
Adopting these strategies will strengthen our response to azithromycin resistance and safeguard public health. Continuous monitoring and research will create a proactive framework for tackling this urgent issue effectively.