Women with clotting disorders should approach the use of Clomid with caution. Clomid is often prescribed to enhance ovulation, but its impact on clotting factors can pose significant risks. If you have a known clotting disorder such as Factor V Leiden or antiphospholipid syndrome, consult with your healthcare provider before starting treatment.
Studies show that certain medications, including Clomid, can potentially increase the risk of thromboembolic events in predisposed individuals. Ensure that your doctor is fully aware of your medical history, including any blood clotting issues, to tailor the treatment approach effectively.
Regular monitoring during Clomid therapy is key. Healthcare professionals may recommend additional tests to evaluate your clotting status throughout the treatment cycle. Maintaining open communication with your healthcare team will help manage any risks associated with Clomid and clotting disorders.
Being informed empowers you to make decisions that prioritize your health. Understanding the potential implications of Clomid on clotting factors will guide you to safer choices in your fertility journey.
- Clomid and Clotting Disorder: A Comprehensive Overview
- Understanding Clomid
- Clotting Disorders Overview
- Understanding Clomid: Mechanism and Uses
- Clotting Disorders: Types and Implications for Fertility
- Types of Clotting Disorders
- Implications for Fertility
- The Impact of Clomid on Patients with Clotting Disorders
- Assessing Risks and Benefits
- Monitoring and Management Strategies
- Best Practices for Managing Clomid Treatment in Patients with Clotting Issues
Clomid and Clotting Disorder: A Comprehensive Overview
Women with clotting disorders should approach Clomid therapy with caution due to potential risks associated with ovulation induction. Research indicates that Clomid may lead to increased thromboembolic events in some patients. Prior to starting treatment, thorough evaluation of blood-clotting profiles is recommended.
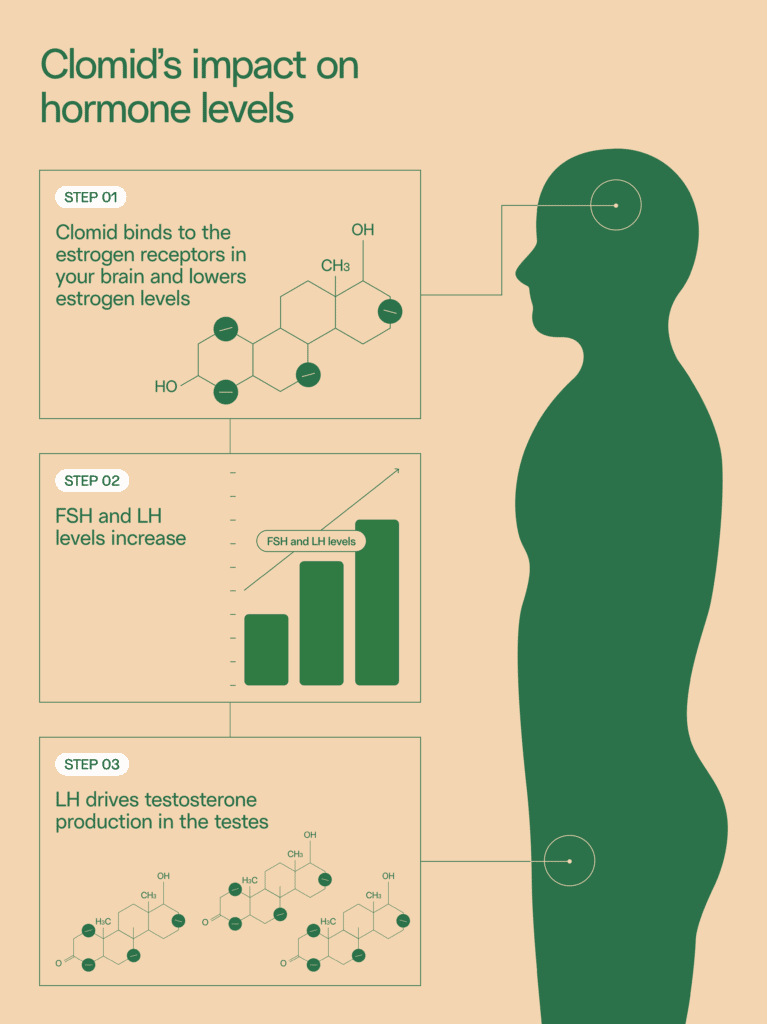
Understanding Clomid
Clomid, or clomiphene citrate, is a medication commonly used to treat infertility by stimulating ovulation. It works by blocking estrogen receptors in the hypothalamus, leading to an increase in the release of gonadotropins, which promote follicle development and ovulation. However, its impact on women with clotting disorders necessitates careful consideration.
Clotting Disorders Overview
Clotting disorders, such as Factor V Leiden, antiphospholipid syndrome, or prothrombin gene mutation, can increase the risk of deep vein thrombosis (DVT) and pulmonary embolism (PE). These conditions may lead to serious complications, especially during pregnancy. Here are key points to consider:
- Consult a hematologist before starting Clomid.
- Consider alternative fertility treatments that may pose lower risks for clotting issues.
- Monitor for symptoms of thrombosis such as swelling, pain in the leg, or shortness of breath.
- Discuss potential prophylactic anticoagulation therapy with your healthcare provider if Clomid is prescribed.
Ultimately, individualized care is crucial. Continuous monitoring and open communication with your healthcare team will support safe and effective treatment planning.
Understanding Clomid: Mechanism and Uses
Clomid, or clomiphene citrate, works by stimulating the pituitary gland to release hormones that promote ovarian follicle growth and ovulation. This medication acts as a selective estrogen receptor modulator (SERM), which means it can block estrogen in some tissues while stimulating it in others. Its primary use is in treating female infertility, particularly in cases of anovulation or irregular ovulation.
Patients typically take Clomid in pill form for five days during the menstrual cycle. Monitoring through blood tests and ultrasounds ensures proper response and dosage adjustments if necessary. Clomid’s effectiveness varies, and it is crucial to follow up with a healthcare provider regularly to assess progress and manage any side effects.
Common indications for Clomid include:
| Indication | Description |
|---|---|
| Anovulation | Clomid is often prescribed to stimulate ovulation in women who do not regularly ovulate. |
| Polycystic Ovary Syndrome (PCOS) | It helps women with PCOS who experience difficulty in conceiving due to hormonal imbalance. |
| Secondary Infertility | Clomid may be indicated for women who have had successful pregnancies but are now having difficulty conceiving again. |
While Clomid is beneficial, it may lead to side effects such as hot flashes, mood swings, and ovarian hyperstimulation syndrome (OHSS). Healthcare providers often weigh these risks against the benefits when recommending Clomid, particularly in patients with pre-existing conditions that may affect clotting.
Monitoring is essential for those with clotting disorders. Clomid’s impact on hormone levels can interact with coagulation pathways, so discussing personal medical history with a provider is crucial for safe use.
In conclusion, understanding Clomid’s mechanism and appropriate applications can optimize treatment strategies for those facing infertility challenges while considering individual health profiles and risks.
Clotting Disorders: Types and Implications for Fertility
Women with clotting disorders should investigate their reproductive options thoroughly. Various clotting disorders can significantly impact fertility and pregnancy outcomes.
Types of Clotting Disorders
The most common types include:
- Antiphospholipid Syndrome (APS): This autoimmune condition increases the risk of blood clots and may lead to pregnancy complications such as miscarriage or preeclampsia.
- Factor V Leiden: This genetic mutation heightens the risk of clotting, which can influence assisted reproductive technologies and pregnancy management.
- Prothrombin Gene Mutation: Similar to Factor V Leiden, this mutation can increase thrombosis risk.
- Protein C Deficiency: This hereditary disorder may also affect fertility and can complicate pregnancy.
- Protein S Deficiency: Another hereditary condition that can cause blood clot formation and is crucial to consider when planning for pregnancy.
Implications for Fertility
Understanding these conditions is vital for developing a tailored approach to fertility. Women with clotting disorders may face increased challenges such as:
- Higher Miscarriage Rates: Many women experience more frequent miscarriages, particularly in the first trimester.
- Increased Need for Monitoring: Close observation by healthcare providers becomes necessary throughout pregnancy to manage clotting risks effectively.
- Influence on Fertility Treatments: Clotting disorders may necessitate adjustments in protocols for treatments like IVF, including anticoagulant therapy.
It is crucial for women with these disorders to collaborate with hematologists and fertility specialists. They can optimize treatment strategies and monitor health to enhance reproductive outcomes.
The Impact of Clomid on Patients with Clotting Disorders
Clomid (clomiphene citrate) can influence individuals with clotting disorders, and medical professionals should evaluate risk factors before prescribing it. Patients with conditions like Factor V Leiden or antiphospholipid syndrome might face increased risks of thromboembolic events due to hormonal changes. Regular blood tests to monitor coagulation levels are recommended during treatment.
Assessing Risks and Benefits
Before initiating Clomid therapy, a thorough assessment of the patient’s clotting history is essential. For those with a known clotting disorder, alternatives to Clomid might be safer options. Should Clomid be prescribed, close monitoring during the first few cycles helps manage any complications that may arise.
Monitoring and Management Strategies
Patients should have routine check-ins with healthcare providers to evaluate their response to Clomid. Encourage open communication about any symptoms that may indicate blood clot formation, such as unexplained leg swelling or severe headaches. Implementing a proactive management plan, potentially involving anticoagulant therapy, can minimize risks and maximize reproductive outcomes.
Best Practices for Managing Clomid Treatment in Patients with Clotting Issues
Regular monitoring of the patient’s clotting parameters is crucial throughout Clomid therapy. Schedule routine blood tests to assess coagulation levels and adjust treatment as needed.
Consider a thorough review of the patient’s medical history. Identify any past incidents of thromboembolic events and current medications that may interfere with coagulation. Maintain open communication with healthcare providers involved in the patient’s care.
Encourage patients to stay hydrated. Adequate hydration can help maintain blood viscosity, reducing the risk of clot formation during treatment.
Advise patients about recognizing early signs of thrombosis, such as swelling, pain, or changes in skin color in the extremities. Prompt reporting of these symptoms can lead to timely intervention.
To optimize treatment safety, collaborate with a hematologist when necessary. Their expertise can guide adjustments in Clomid dosages or suggest alternative fertility therapies if risks are deemed high.
Encourage patients to follow a balanced diet rich in omega-3 fatty acids, antioxidants, and fibers. These nutritional components can support vascular health and may aid in reducing clotting risks.
Educate patients on lifestyle modifications, such as engaging in light physical activity, which promotes circulation and helps manage weight. Encourage them to avoid prolonged periods of immobility, particularly during Clomid treatment.
Reassess the treatment plan if patients experience side effects, particularly those related to blood clotting. Regular check-ins can help identify issues early and adjust the approach accordingly.
Maintain a consistent follow-up schedule to monitor the patient’s response to Clomid. This can enhance the safety and effectiveness of the treatment plan while accommodating any concerns related to clotting disorders.