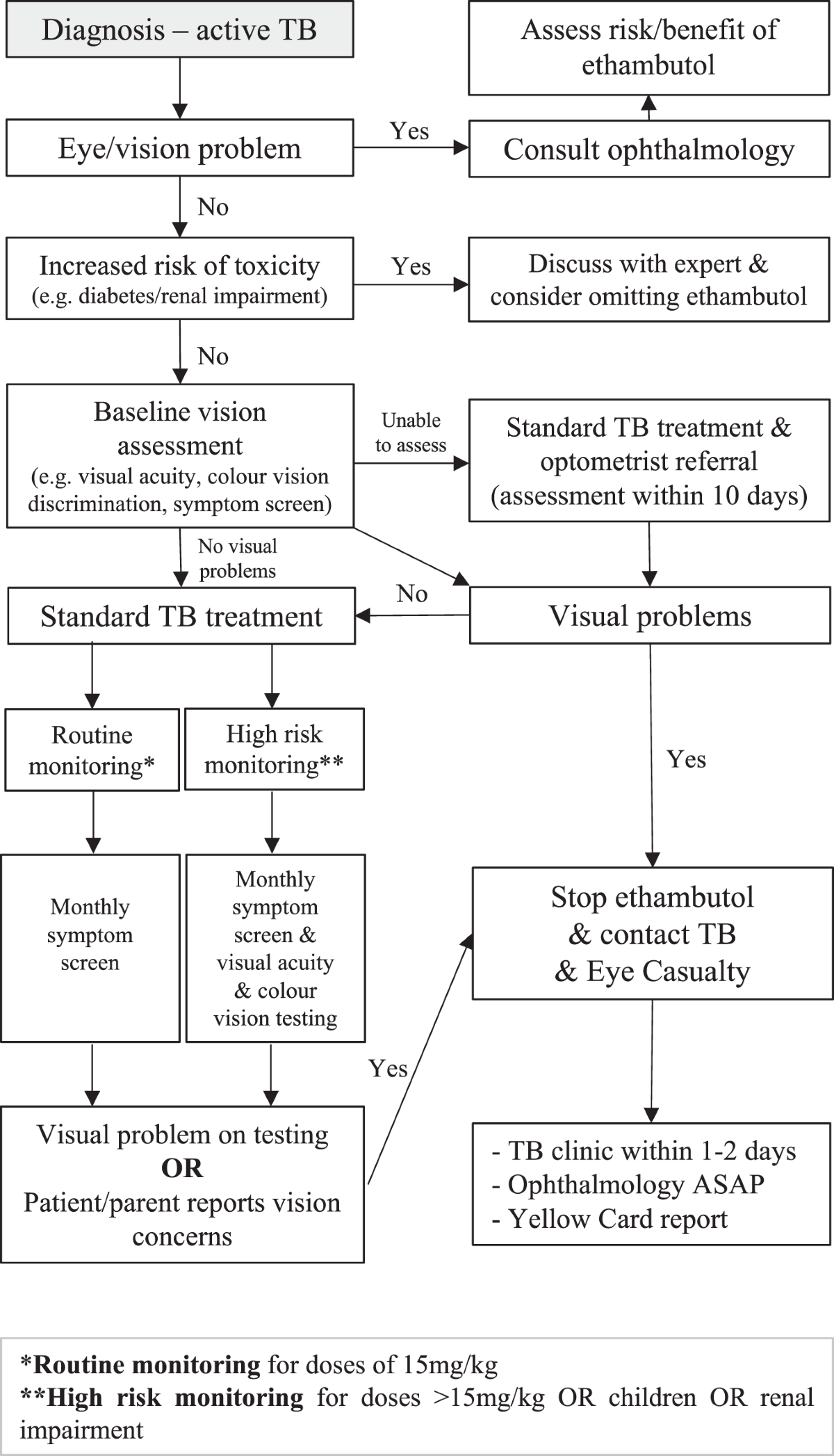
Ophthalmology screening for patients on ethambutol should be conducted routinely to detect potential ocular toxicity early. Ethambutol, primarily used in the treatment of tuberculosis, can lead to adverse effects such as vision impairment and optic neuritis. Regular eye examinations enable healthcare providers to monitor any signs of these complications effectively.
Begin screening within the first month of ethambutol therapy and continue assessments every month for the initial three months. Following this period, transitioning to a quarterly schedule is advisable, provided no symptoms arise. If patients report any visual disturbances–such as blurred vision, changes in color perception, or scotomas–an immediate ophthalmological evaluation is warranted.
Incorporating visual acuity tests and color vision assessments into the screening protocol is critical. Consider utilizing the Ishihara test for color discrimination to spot early signs of toxicity. Education on possible symptoms should also be provided to patients, ensuring they understand when to seek help. This proactive approach safeguards against irreversible damage and enhances patient outcomes.
- Ethambutol Ophthalmology Screening: A Comprehensive Overview
- Screening Protocol Recommendations
- Monitoring and Patient Education
- Understanding Ethambutol: Mechanism and Uses
- Importance of Ophthalmology Screening in Ethambutol Therapy
- Key Recommendations for Screening
- Symptoms to Monitor
- Key Visual Symptoms Indicative of Ethambutol Toxicity
- Recommended Protocols for Ethambutol-Related Eye Screenings
- Best Practices for Documenting and Reporting Screening Results
- Future Directions in Ethambutol Ophthalmology Screening Research
- Integration of Advanced Imaging Techniques
- Patient-Centric Approaches
Ethambutol Ophthalmology Screening: A Comprehensive Overview
Regular ophthalmology screenings are critical for patients receiving Ethambutol therapy. Ethambutol, known for its use in treating tuberculosis, can lead to progressive optic neuropathy, impacting visual acuity and color perception. Implementing a standardized screening protocol helps in early detection and management of these potential side effects.
Screening Protocol Recommendations
Start with a baseline visual acuity assessment. Document both distance and near vision in each eye using standard charts. Follow up with color vision testing, employing the Ishihara test to identify any red-green color deficiencies, which may indicate Ethambutol-related toxicity. Regular follow-up examinations should occur every month during the initial treatment phase and every three months thereafter, or sooner if symptoms arise.
Monitoring and Patient Education
Educate patients about symptoms to watch for, such as blurred vision, changes in color perception, or discomfort. Encourage them to report any visual disturbances promptly. In cases of detected toxicity, consider discontinuing Ethambutol and consult with a specialist for potential management strategies. Sustained outreach and support ensure that patients remain informed and engaged in their ophthalmic health while on therapy.
Understanding Ethambutol: Mechanism and Uses
Ethambutol works by inhibiting the synthesis of the bacterial cell wall, specifically targeting the arabinogalactan layer. This mechanism disrupts the integrity of the cell wall, leading to the death of Mycobacterium tuberculosis. By blocking the enzyme arabinosyl transferase, Ethambutol effectively reduces the production of polysaccharides essential for bacterial growth.
Clinicians primarily prescribe Ethambutol for the treatment of pulmonary tuberculosis, often in combination with other anti-tuberculous agents to enhance efficacy. This multidrug approach helps to prevent resistance development. Ethambutol is especially valuable in cases where resistance to first-line drugs is suspected or confirmed, as it shows activity against many resistant strains.
While using Ethambutol, regular ophthalmic screening becomes fundamental due to potential side effects, particularly optic neuritis, which can lead to vision impairment. Patients should have baseline visual acuity assessments before initiating treatment, along with periodic checks during therapy. Early detection of visual changes enables timely intervention, minimizing long-term complications.
In addition to treating tuberculosis, ongoing studies are exploring Ethambutol’s role in other infections, such as certain bacterial and fungal diseases, though its primary indication remains in tuberculosis management. Understanding its therapeutic uses, along with monitoring for adverse effects, is vital for optimizing patient outcomes.
Importance of Ophthalmology Screening in Ethambutol Therapy
Regular ophthalmology screening is crucial for patients undergoing Ethambutol therapy. Ethambutol, an antibiotic primarily used for tuberculosis treatment, can cause ocular toxicity, leading to vision impairment if not monitored properly. Conducting eye examinations before and during treatment allows for early detection of potential side effects.
Key Recommendations for Screening
The American Academy of Ophthalmology suggests that patients receiving Ethambutol should have a comprehensive eye examination prior to starting the treatment. Continuous monitoring every one to three months during therapy is advisable, particularly for those taking doses higher than 15 mg/kg/day.
| Screening Interval | Action Required |
|---|---|
| Before Treatment | Complete eye exam to assess baseline vision. |
| Monthly During Therapy | Visual acuity testing to monitor changes. |
| Post-Treatment | Follow-up exam to evaluate recovery of vision. |
Symptoms to Monitor
Patients should be educated about symptoms indicating potential ocular issues, such as blurred vision, changes in color perception, or loss of visual acuity. Immediate reporting of these symptoms can lead to timely intervention and prevent lasting damage.
By prioritizing regular ophthalmology screenings, healthcare providers can ensure that patients maintain visual health while benefiting from Ethambutol therapy. Monitoring not only enhances patient safety but also contributes to treatment adherence and overall effectiveness.
Key Visual Symptoms Indicative of Ethambutol Toxicity
Monitor for visual disturbances such as blurred vision, which often indicates ethambutol toxicity. Patients may also report color vision changes, particularly difficulties in distinguishing red and green shades. These symptoms arise from optic neuropathy linked to the drug.
Assess for central scotomas, where patients notice blind spots or diminished vision in their central field. This symptom can significantly impact daily activities. Regular visual acuity tests are recommended for early detection of any impairment.
Look out for any signs of visual field defects during eye examinations. These may manifest as constricted peripheral vision, which is critical to identify before irreversible damage occurs.
Conduct thorough dilated fundus examinations to check for abnormalities in the optic nerve head. Swelling or pallor of the optic disc may suggest ongoing toxicity and should prompt a reevaluation of the patient’s medication regimen.
Instruct patients to report any sudden onset of vision changes as these could indicate acute toxicity. Evaluate any visual complaints promptly, as timely interventions can mitigate potential complications associated with ethambutol use.
Recommended Protocols for Ethambutol-Related Eye Screenings
Conduct an initial ophthalmologic examination before initiating ethambutol treatment. This screening should include visual acuity tests, color vision testing, and a dilated fundus examination to establish a baseline.
Schedule regular follow-up eye examinations every month during the first three months of treatment. If no adverse effects are identified, extend the interval to every three months thereafter. Early detection of ethambutol-related adverse effects is crucial.
Incorporate specific color vision testing using pseudoisochromatic plates, such as the Ishihara test, at each follow-up visit. Monitor for any signs of color vision deficiency, which can indicate potential toxicity.
Educate patients on visual symptoms that warrant immediate reporting, such as changes in vision, color perception, or signs of eye discomfort. Ensure they understand the importance of promptly addressing these concerns.
Use optical coherence tomography (OCT) for patients at higher risk of developing eye complications due to coexisting conditions. This imaging technique can help in monitoring retinal changes associated with ethambutol.
Maintain detailed records of each screening, documenting findings and any changes in visual function or symptoms. This helps to track patient progress and modify treatment plans when necessary.
Collaborate with pharmacists to ensure patients receive clear guidance on the importance of adhering to the prescribed dosage of ethambutol. Proper adherence minimizes the risk of visual side effects.
Consider referral to an ophthalmologist if any visual impairment or symptoms arise during treatment. Early intervention can prevent long-term damage to the eyes.
Best Practices for Documenting and Reporting Screening Results
Maintain clear and consistent formats for documenting screening results. Standardized templates streamline data entry and enhancements in readability.
- Use Specific Terminology: Utilize precise medical terms to avoid ambiguity. Clarify findings such as “color vision deficiency” instead of vague terms like “vision problem.”
- Include Patient Information: Record essential details: patient ID, age, gender, and medical history. This data contextualizes the results for future reference.
- Document Screening Date: Always note the date of the screening for tracking patient progress and regulatory purposes. Include follow-up dates if applicable.
- Be Thorough in Descriptions: Describe findings comprehensively. For example, detail the nature of any abnormalities detected during screening.
Reporting findings involves clear communication with healthcare providers and patients.
- Summarize Key Findings: Provide a concise overview of the most critical results at the beginning of the report.
- Use Visual Aids: Present charts or graphs for trends or significant data points. This visual support enhances understanding.
- Follow Up on Abnormal Results: Establish a protocol for notifying patients about abnormal screenings and outlining subsequent steps clearly.
Ensure secure data handling practices. Protect patient information with confidentiality measures to comply with relevant regulations.
Regularly review and update documentation practices to adapt to best standards in ophthalmology screening. Engaging the team in this process fosters accountability and continuous improvement.
Future Directions in Ethambutol Ophthalmology Screening Research
Enhancing screening protocols for ethambutol-related ocular toxicity stands at the forefront of upcoming research. Researchers should develop criteria for monitoring visual acuity and color discrimination earlier in treatment regimens, particularly in high-risk populations. These criteria would allow for timely intervention before irreversible damage occurs.
Integration of Advanced Imaging Techniques
Adopting advanced imaging modalities such as optical coherence tomography (OCT) can significantly improve the detection of retinal changes associated with ethambutol use. Incorporating these technologies into routine screening could reveal subtle retinal shifts that traditional methods might miss. Studies focusing on establishing baseline retinal thickness and changes during treatment will provide valuable insights.
Patient-Centric Approaches
Implementing patient-reported outcome measures can contribute to a more holistic understanding of ethambutol’s impact on vision. Surveys focused on visual symptoms, quality of life, and satisfaction with ocular health services can guide practitioners in personalizing care. Further research into the psychological effects of potential vision loss can enhance support and management frameworks for patients undergoing treatment.