For individuals dealing with intestinal motility disorders, the recommended dosage of Diflucan (fluconazole) typically starts at 150 mg once, followed by 150 mg weekly for maintenance, depending on the medical condition being treated. Always consult a healthcare provider to tailor the dosage to specific health needs and conditions.
Diflucan effectively addresses fungal infections that can complicate motility disorders, as a compromised gut may lead to overgrowth of harmful microorganisms. Adjusting the dosage may be necessary based on individual response, underlying health issues, and potential interactions with other medications.
Monitoring is critical when using Diflucan for intestinal issues. Regular follow-ups with a healthcare professional ensure the treatment remains safe and effective. If gastrointestinal symptoms aggravate or new symptoms develop, communication with the prescribing doctor should occur immediately to reevaluate the treatment plan.
- Intestinal Motility Disorder and Diflucan Dosage
- Understanding Intestinal Motility Disorders
- Mechanism of Action of Diflucan in Gut Health
- Impact on Gut Flora
- Inflammation Reduction
- Recommended Dosage of Diflucan for Intestinal Motility Disorders
- Factors Influencing Diflucan Dosage Adjustments
- Potential Side Effects of Diflucan in Patients with Motility Issues
- Gastrointestinal Symptoms
- Drug Interactions
- Clinical Guidelines for Monitoring Patients on Diflucan
- Assessing Drug Interactions
- Patient Monitoring for Adverse Effects
Intestinal Motility Disorder and Diflucan Dosage
For individuals with intestinal motility disorders, the standard dose of Diflucan (fluconazole) typically ranges from 150 mg to 400 mg based on the specific condition being treated. Monitor symptoms closely during treatment.
Consider the following recommendations when administering Diflucan:
- Baseline Assessment: Evaluate renal function prior to starting therapy, as dosage adjustments may be necessary for patients with impaired renal function.
- Monitoring: Regularly assess liver enzyme levels and renal function during treatment to identify any potential adverse effects early.
- Duration: Treatment duration can vary; acute infections often require 2 to 4 weeks, while chronic infections may necessitate longer treatment courses.
- Drug Interactions: Review any concurrent medications to avoid potential interactions that might affect drug metabolism or increase toxicity.
For patients struggling with symptoms of gastrointestinal disturbance, consider supportive care alongside antifungal treatment. This may include:
- Dietary modifications to alleviate symptoms.
- Regular hydration to minimize complications.
- Probiotics to help restore intestinal flora.
Consult healthcare providers regularly to assess treatment effectiveness and symptom improvement. Adjustments in dosage may be necessary, particularly for individuals with persistent gastrointestinal symptoms or those experiencing side effects.
Understanding Intestinal Motility Disorders
Intestinal motility disorders disrupt the normal movement of the digestive tract. Frequency and rhythm of contractions can either increase or decrease, leading to symptoms such as bloating, constipation, or diarrhea. These disorders include conditions like irritable bowel syndrome (IBS), gastroparesis, and intestinal pseudo-obstruction.
Effective management starts with identifying the specific disorder. For IBS, dietary changes like low FODMAP diets may alleviate symptoms. In cases of gastroparesis, small, frequent meals and low-fiber foods can ease the burden on the stomach. Prokinetic agents might also be considered to enhance gastric emptying.
Hydration remains key. Staying well-hydrated can support gut function. Use of electrolyte solutions can further assist where diarrhea is present.
Monitoring fiber intake is crucial. Soluble fiber, found in oats and fruits, can help manage symptoms, while insoluble fiber might worsen bloating for some individuals. Tailoring fiber intake to personal tolerance plays a significant role in symptom relief.
Medications can provide additional support. Antispasmodics can relieve cramping, while laxatives may be necessary for constipation. Always consult a healthcare provider before starting any new medication.
Regular physical activity contributes positively to intestinal health. Even light exercise, such as walking, encourages normal gut motility and can reduce severity of symptoms.
Cognitive-behavioral therapy (CBT) may benefit those with associated anxiety or stress. Addressing the psychological aspects can lead to improved management of physical symptoms.
Finally, ongoing communication with healthcare professionals ensures tailored treatment plans that adapt as needs evolve. Taking proactive steps in understanding and managing intestinal motility disorders can lead to improved quality of life.
Mechanism of Action of Diflucan in Gut Health
Diflucan, or fluconazole, functions primarily as an antifungal agent, targeting Candida species and other fungi in the intestines. It achieves this by inhibiting the enzyme lanosterol demethylase, critical in the synthesis of ergosterol, a key component of fungal cell membranes. By disrupting the integrity of these membranes, Diflucan effectively reduces fungal proliferation in the gut.
Impact on Gut Flora
Maintaining a balanced gut microbiome is essential for overall health. Diflucan selectively targets pathogenic fungi while sparing beneficial bacteria. This selective action helps prevent the overgrowth of harmful organisms, contributing to a healthier gut environment. Research indicates that restoring balance in gut flora can enhance digestion and nutrient absorption.
Inflammation Reduction
Diflucan may also play a role in mitigating inflammation within the gastrointestinal tract. By reducing fungal load, it helps alleviate inflammation associated with conditions like candidiasis, which can lead to symptoms such as bloating, pain, and irregular motility. Keeping inflammation in check supports better gut motility and overall digestive comfort.
In conclusion, Diflucan operates effectively by targeting fungal organisms, supporting gut flora balance, and reducing inflammation. These mechanisms combine to promote gut health, making it a valuable option for addressing intestinal motility disorders attributed to fungal overgrowth.
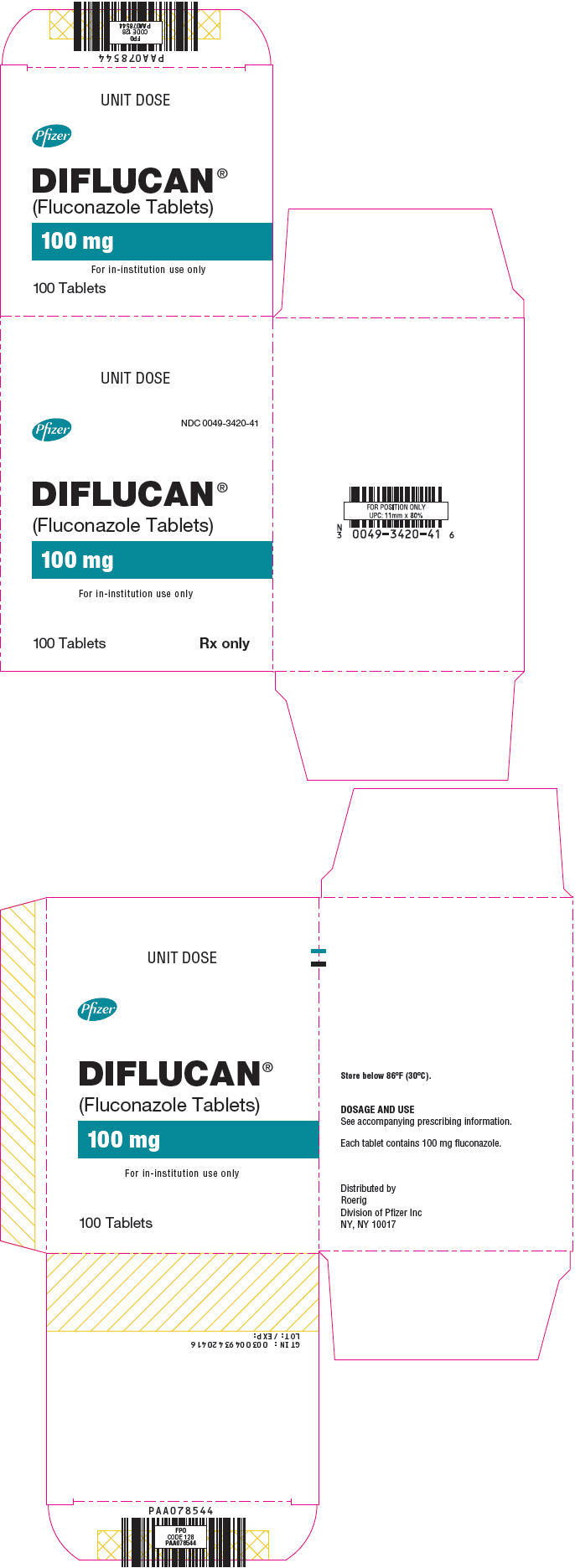
Recommended Dosage of Diflucan for Intestinal Motility Disorders
The standard dosage of Diflucan (flucoconazole) for treating intestinal motility disorders is typically 200 mg on the first day, followed by 100 mg daily for at least two weeks. This regimen helps combat fungal infections that may contribute to motility issues.
For severe infections or compromised immune systems, healthcare providers may increase the dose to 400 mg on the first day, followed by 200 mg or more daily, based on clinical response. Tailoring the dosage is common in clinical practice to achieve the desired therapeutic outcomes.
Patients should maintain regular follow-ups to monitor liver function and any potential side effects. Adjustment of the dosage may be necessary if the patient experiences adverse effects or if there is a poor clinical response to the initial regimen.
Always consult a healthcare professional before starting or adjusting any medication. Below is a summary of recommended dosages:
| Condition | Initial Dose | Maintenance Dose |
|---|---|---|
| Intestinal Motility Disorders | 200 mg on Day 1 | 100 mg daily thereafter |
| Severe Infections | 400 mg on Day 1 | 200 mg or more daily based on response |
Regular assessment is key to ensuring safety and efficacy during treatment. Adjustments made during these evaluations can lead to better patient outcomes.
Factors Influencing Diflucan Dosage Adjustments
Consider the patient’s kidney function when adjusting Diflucan dosages. Renal impairment can lead to decreased clearance of the drug, necessitating reductions in dosage to avoid toxicity. Regular monitoring of renal parameters is advisable for accurate adjustments.
Assess liver function as well. Liver disease can impact drug metabolism, potentially modifying the required dosage. Patients with hepatic impairment may require dosage adjustments to ensure therapeutic efficacy while minimizing adverse effects.
Evaluate the patient’s age. Elderly patients often exhibit altered pharmacokinetics, warranting careful consideration of dosage. Reduced renal and hepatic function, along with polypharmacy issues, can make dosage adjustments beneficial.
Take into account the type and severity of the infection being treated. More severe or resistant fungal infections typically demand higher doses, while uncomplicated cases may require less. Tailor dosages based on clinical response and laboratory findings.
Monitor concomitant medications. Drug interactions can elevate or decrease Diflucan levels, necessitating dosage modification. Always review the patient’s medication list for potential interactions that could impact treatment outcomes.
Consider individual patient factors such as genetic variations in drug metabolism. Pharmacogenomic testing can provide valuable insights and guide personalized dosing regimens based on metabolism profiles.
Lastly, observe for clinical symptoms and side effects during treatment. If adverse effects arise, reassess the dosage and consider whether a lower dose or a different antifungal agent may be more appropriate. Continuously adapt treatment based on the patient’s response to therapy.
Potential Side Effects of Diflucan in Patients with Motility Issues
Patients with intestinal motility disorders should monitor for specific side effects when taking Diflucan (fluconazole). Gastrointestinal symptoms often arise, including nausea, diarrhea, and abdominal pain. These effects may exacerbate existing motility concerns, leading to heightened discomfort or other complications.
Gastrointestinal Symptoms
Nausea and vomiting can occur in some individuals. These symptoms may worsen underlying motility problems, potentially impacting fluid and nutrient absorption. Diarrhea, another common side effect, can lead to dehydration, especially in those with pre-existing motility disorders. It’s crucial to assess hydration levels regularly and adjust intake accordingly.
Drug Interactions
Diflucan may interact with other medications commonly used by patients with motility issues. For instance, combining it with certain proton pump inhibitors or antacids can alter the effectiveness of both drugs. Always consult a healthcare provider to review all medications to minimize adverse interactions.
Staying attentive to these potential side effects ensures better management of health conditions while on Diflucan. Regular communication with a healthcare professional is advisable to address any concerns or modify treatment as necessary.
Clinical Guidelines for Monitoring Patients on Diflucan
Monitor liver function tests (LFTs) before initiating Diflucan therapy and periodically during treatment. Check LFTs at baseline, two weeks after starting the drug, and every month thereafter, especially in patients with pre-existing liver conditions or those on concurrent hepatotoxic medications.
Assessing Drug Interactions
Review patient’s medication history for potential drug interactions. Diflucan can increase the plasma levels of various medications, such as certain antiepileptics and anticoagulants. Consider monitoring plasma levels of these drugs more closely during and after initiation of Diflucan therapy.
Patient Monitoring for Adverse Effects
- Advise patients to report any signs of liver dysfunction, including jaundice, dark urine, or extreme fatigue.
- Monitor for skin reactions, such as rash or itching, as this could indicate hypersensitivity.
- Evaluate for any gastrointestinal symptoms, including nausea, vomiting, or abdominal pain, which could suggest intolerance or adverse effects.
Counsel patients to adhere strictly to prescribed dosages. If a dose is missed, they should take it as soon as possible unless it is close to the time for the next dose. In such cases, the missed dose should be skipped.
Periodic assessment of symptom relief or resolution of the underlying infection is necessary to evaluate treatment effectiveness. Adjust the treatment regimen based on clinical response and laboratory findings.
Provide clear instructions regarding the importance of completing the full course of therapy, even if symptoms improve before the medication is finished. This helps prevent recurrence and resistance development.