Neurontin, commonly known as gabapentin, shows promising results in managing movement disorders, particularly in patients experiencing symptoms of essential tremor and dystonia. Clinicians often prescribe it off-label as an adjunct therapy due to its ability to stabilize neuronal excitability.
Research indicates that gabapentin can help alleviate symptoms by modulating neurotransmitter release. In studies with patients suffering from movement disorders, doses typically range from 300 mg to 2400 mg per day, allowing for individualized treatment. Adjusting the dosage based on patient response can enhance therapeutic outcomes while minimizing potential side effects.
Regular monitoring is crucial for those using Neurontin. Side effects such as dizziness or fatigue may occur, yet many patients report improved quality of life and reduced severity of symptoms. Collaborative discussions with healthcare providers regarding the treatment plan ensure that adjustments are made as necessary to maximize benefits.
Incorporating Neurontin into a comprehensive treatment plan that includes physical therapy and lifestyle modifications can yield positive results for those with movement disorders. Patients are encouraged to maintain open lines of communication with their medical team to navigate challenges effectively.
- Neurontin for Movement Disorder
- Understanding Movement Disorders and Their Impact
- Symptoms and Types
- Treatment Options and Approach
- What is Neurontin (Gabapentin)?
- Mechanism of Action of Neurontin in Movement Disorders
- Calcium Channel Interaction
- Impact on GABAergic Transmission
- Clinical Evidence Supporting Neurontin for Movement Disorders
- Dosage Guidelines and Administration of Neurontin
- Potential Side Effects and Risks of Neurontin
- Less Common but Serious Risks
- Long-term Considerations
- Comparing Neurontin with Other Treatment Options
- Patient Experiences and Case Studies with Neurontin
- Long-term Use and Adjustments
- Combination Therapies
Neurontin for Movement Disorder
Using Neurontin (gabapentin) for movement disorders can provide significant relief for some patients. It is particularly helpful for those experiencing tremors, dystonia, and other involuntary movements. Cognizant of the individual response to treatment, it’s advisable to consult with a healthcare provider for personalized dosage recommendations.
Clinical studies indicate that Neurontin may help reduce the severity and frequency of movement symptoms. This medication acts on GABA receptors, promoting a calming effect on neural pathways, which can be beneficial for various movement disorders.
Consider these points when assessing Neurontin for movement disorders:
- Dosage: Start with a low dose, gradually increasing to minimize side effects.
- Side Effects: Be alert for dizziness, fatigue, and coordination issues. Monitor how these affect daily activities.
- Drug Interactions: Inform your doctor about all medications taken, as interactions can affect Neurontin’s effectiveness.
- Monitor Progress: Regular check-ins with your provider are essential to evaluate symptom improvement and medication tolerance.
Some patients report positive outcomes with Neurontin as a monotherapy, while others may find it beneficial as an adjunct to other treatments. Discuss the potential for combination therapy with your healthcare provider to tailor the approach to your specific needs.
Always consider lifestyle factors such as stress management and physical therapy, which may enhance the effectiveness of Neurontin in managing movement disorders.
In summary, Neurontin can be an effective option, yet individualized treatment plans are crucial for optimal results. Engage in open communication with your healthcare team to find the best therapeutic strategy.
Understanding Movement Disorders and Their Impact
Movement disorders significantly affect daily life, manifesting through tremors, rigidity, or involuntary movements. These conditions challenge coordination, balance, and fine motor skills, leading to difficulties in routine activities such as writing, eating, or walking.
Symptoms and Types
Common movement disorders include Parkinson’s disease, essential tremor, dystonia, and Huntington’s disease. Each presents unique symptoms: Parkinson’s often leads to a shuffling gait and resting tremors, while essential tremor primarily involves shaking hands. Understanding these symptoms helps in recognizing the need for early intervention.
Treatment Options and Approach
While there’s no cure for many movement disorders, various treatment options aim to manage symptoms. Medications such as Neurontin (gabapentin) have shown promise in reducing certain movement-related issues. Physical therapy, occupational therapy, and lifestyle adjustments also play a significant role in enhancing quality of life. Regular consultations with healthcare providers ensure tailored treatment plans to address individual needs.
Awareness and education about movement disorders empower patients and caregivers, fostering a proactive approach to management and support. Sharing experiences within communities can provide relief and practical strategies, encouraging a more fulfilling life despite challenges.
What is Neurontin (Gabapentin)?
Neurontin, known by its generic name gabapentin, is a medication primarily prescribed for neuropathic pain and as an adjunct therapy for seizures. It acts by stabilizing electrical activity in the brain and influencing neurotransmitter release, which helps in reducing pain and seizure frequency. Patients with movement disorders may benefit from gabapentin due to its effects on nerve signaling.
This medication is available in various forms, including capsules, tablets, and oral solutions. Doctors typically recommend a gradual increase in dosage to minimize side effects and to determine the optimal therapeutic level for each patient. Common side effects include drowsiness, dizziness, and fatigue, which may lessen as the body adjusts to the treatment.
Clinical studies indicate that gabapentin may provide symptomatic relief for individuals experiencing tremors or other movement-related issues. It is particularly useful for those with conditions linked to nerve dysfunction. However, patients should consult healthcare providers to ensure that gabapentin is appropriate for their specific situation, especially if they are taking other medications.
Regular follow-ups with the prescribing physician can help monitor any side effects and assess treatment effectiveness. Adjustments to dosage and medication can be made based on the patient’s response. Always discuss any concerns or new symptoms that arise during treatment.
Mechanism of Action of Neurontin in Movement Disorders
Neurontin, also known as gabapentin, exerts its therapeutic effects primarily by modulating the release of excitatory neurotransmitters through its action on voltage-gated calcium channels. This mechanism plays a significant role in reducing synaptic transmission that is often hyperactive in various movement disorders.
Calcium Channel Interaction
Specifically, Neurontin binds to the α2δ subunit of these calcium channels in the central nervous system. This results in decreased influx of calcium ions during neuronal depolarization. By inhibiting this process, Neurontin effectively dampens excessive neurotransmitter release, particularly glutamate, which is frequently implicated in hyperexcitability and movement disorders.
Impact on GABAergic Transmission
Although Neurontin does not directly enhance GABA levels, it indirectly modifies GABAergic transmission. The reduction of glutamate release leads to an increase in relative GABAergic activity, promoting inhibitory signaling. This effect helps stabilize neural circuits that may otherwise contribute to tremors or involuntary movements.
| Mechanism | Description |
|---|---|
| Calcium Channel Modulation | Binds to α2δ subunit, reducing calcium influx and excitatory neurotransmitter release. |
| GABAergic Influence | By decreasing glutamate, it enhances GABAergic activity, stabilizing neural circuits. |
This dual action of Neurontin provides a beneficial effect for patients experiencing movement disorders, leading to improved control over symptoms and enhancing overall quality of life. As the understanding of its mechanism deepens, more targeted approaches to treatment may emerge.
Clinical Evidence Supporting Neurontin for Movement Disorders
Clinical studies demonstrate the efficacy of Neurontin (Gabapentin) in managing various movement disorders. The data highlights specific conditions where Neurontin shows promise.
- Essential Tremor: Research indicates that Neurontin can significantly reduce tremor amplitude. A randomized double-blind trial reported a 50% reduction in tremor severity among participants after 12 weeks of treatment.
- Dystonia: A study involving patients with dystonia revealed that Neurontin administration led to marked improvements in symptom severity. Over a 6-month period, participants noted a substantial decline in episodes.
- Restless Legs Syndrome (RLS): Neurontin has been associated with a decrease in RLS symptoms. One trial demonstrated a notable decrease in the International Restless Legs Scale scores, enhancing overall sleep quality.
Weight gain and sedation are potential side effects of Neurontin, but patient feedback often highlights good tolerance and a favorable safety profile compared to traditional Parkinson’s disease medications.
Dosage adjustments may be necessary based on individual responses. Starting doses often range from 300 mg/day, gradually increasing as needed, while monitoring for efficacy and tolerance.
Ongoing research continues to evaluate Neurontin’s long-term effects on movement disorders. Preliminary results encourage its consideration as a treatment option, especially for patients unresponsive to conventional therapies.
Dosage Guidelines and Administration of Neurontin
Initiate Neurontin therapy with a dosage of 300 mg taken orally on day one. On day two, increase the dosage to 300 mg twice daily. By day three, administer 300 mg three times daily. This titration helps to minimize potential side effects and allows for assessment of the patient’s response.
For movement disorders, the typical maintenance dose varies. Most patients respond well to a range of 900 mg to 1800 mg per day, divided into three doses. Adjustments may be necessary based on individual effectiveness and tolerability.
Monitor renal function regularly, as dosage may require modification in those with compromised kidney function. In patients with creatinine clearance less than 60 mL/min, consider reducing the total daily dose by half or adjusting administration frequency.
Advise patients to take Neurontin with food to enhance absorption. Encourage consistent timing with doses to maintain steady levels of the medication in the bloodstream.
Assess for side effects periodically, including dizziness, fatigue, and ataxia. Instruct patients to report any unusual symptoms. If side effects are pronounced, consider dosage reduction or discontinuation of the medication.
Always consult healthcare professionals before making changes to the dosage regimen, especially for long-term treatment or in combination with other medications. Regular follow-up appointments will aid in evaluating treatment effectiveness and adjusting management plans accordingly.
Potential Side Effects and Risks of Neurontin
Patients using Neurontin (gabapentin) should be aware of possible side effects, as these can impact overall well-being. The most common adverse effects include dizziness and drowsiness, which may affect daily activities. Staying cautious when engaging in activities that require full alertness, like driving, is advisable.
Less Common but Serious Risks
Some individuals may experience mood changes, including anxiety or depression. Monitoring for these symptoms is crucial, especially for those with a history of mental health issues. Allergic reactions, though rare, may manifest as rashes or swelling. Anyone experiencing these symptoms should seek medical attention immediately.
Long-term Considerations
Long-term use of Neurontin has potential implications, including weight gain and peripheral edema (swelling in the extremities). Regular check-ups can help manage these effects. Inform your healthcare provider about any new symptoms or concerns while on this medication. Open communication ensures that adjustments or alternatives can be explored swiftly if needed.
Remaining informed about these side effects empowers patients to make better choices regarding their treatment and overall health management.
Comparing Neurontin with Other Treatment Options
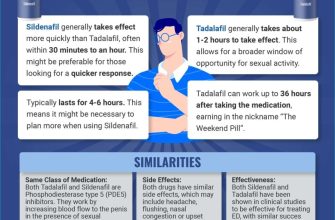
Neurontin (gabapentin) offers a specific advantage in treating movement disorders, particularly those characterized by neuropathic pain or certain types of dyskinesias. Its mechanism, which modulates excitatory neurotransmitters, can lead to symptom relief in many patients.
When comparing Neurontin to other medications such as benzodiazepines, one finds that while benzodiazepines provide rapid calming effects and muscle relaxation, their long-term use raises concerns about dependency and tolerance. Neurontin, on the other hand, generally has a lower potential for abuse and offers a more favorable long-term safety profile.
Dopaminergic agents, widely used in disorders like Parkinson’s disease, can significantly improve motor symptoms but often come with troublesome side effects, such as nausea or dyskinesias. Neurontin can complement these medications by addressing associated pain or discomfort without exacerbating the primary motor symptoms.
Anticonvulsants such as lamotrigine or topiramate are alternatives, targeting different pathways. While these options can be effective, they may not have the same breadth of symptom relief in movement disorders as Neurontin does for some patients. Each patient’s response varies, suggesting that individual trials might be necessary to determine the best fit.
Lastly, physical therapy remains a critical component of movement disorder management. While it does not replace medications, combining Neurontin with a tailored rehabilitation program can enhance outcomes and improve functional capabilities.
In conclusion, Neurontin presents a viable option within a varied treatment regimen for movement disorders. Its unique profile allows it to serve both as a standalone medication and an adjunct to other therapies, thereby broadening treatment possibilities for those affected by these conditions.
Patient Experiences and Case Studies with Neurontin
Patients using Neurontin have reported various outcomes in managing movement disorders. One particularly positive case involved a 45-year-old woman diagnosed with essential tremor. After starting treatment with Neurontin, she noticed a significant reduction in tremor intensity, which allowed her to regain confidence in daily activities such as writing and holding objects. This improvement took about six weeks to manifest, highlighting the need for patience when starting the medication.
Long-term Use and Adjustments
Another case involved a 38-year-old man with dystonia. Initially prescribed a low dose, he experienced mild side effects, including dizziness. His doctor gradually increased the dosage, leading to improved motor control within three months. This gradual titration method proved beneficial, allowing the patient to adapt to Neurontin while minimizing discomfort.
Combination Therapies
Some patients have found success by combining Neurontin with other medications. A 50-year-old woman managing Parkinson’s disease reported that adding Neurontin to her regimen improved her overall quality of life. She noted a decrease in her “off” times and better management of muscle rigidity. This combination highlighted the importance of individualized treatment plans tailored to patients’ unique needs.
Sharing experiences can be invaluable. Connecting with healthcare professionals and support groups can provide insights into managing expectations and optimizing treatment with Neurontin for movement disorders.