If you’re struggling with panic disorder, considering Paxil can lead to significant improvements. This medication, belonging to the class of selective serotonin reuptake inhibitors (SSRIs), often effectively alleviates the symptoms associated with panic attacks. Various studies highlight Paxil’s ability to reduce both the frequency and intensity of these episodes, providing a smoother daily experience for those affected.
When starting treatment with Paxil, it’s essential to consult with a healthcare provider to determine the appropriate dosage tailored to your needs. Many patients begin to notice positive changes within the first few weeks, yet achieving optimal results may take up to 12 weeks. Consistency is key; taking the medication at the same time every day can enhance its effectiveness and help stabilize your mood.
Alongside medication, incorporating therapy can further bolster recovery. Cognitive-behavioral therapy (CBT) has shown promising results for those with panic disorder, offering tools to manage anxiety levels and reduce the fear of future panic attacks. Combining Paxil with therapy creates a holistic approach that can lead to long-term relief.
Monitoring your progress plays a crucial role in treatment. Regular check-ins with your healthcare provider can help evaluate how Paxil is working for you and adjust the plan as needed. Don’t hesitate to share any concerns or side effects experienced during treatment. Open communication can facilitate a more tailored approach, ensuring you receive the best possible care.
- Paxil and Panic Disorder
- Understanding Panic Disorder Symptoms
- Physical Symptoms
- Psychological Symptoms
- The Role of Paxil in Treating Panic Disorder
- Dosage Guidelines for Paxil in Panic Disorder
- Potential Side Effects of Paxil
- Comparing Paxil to Other Treatments for Panic Disorder
- Comparative Effectiveness of SSRIs and Benzodiazepines
- Considerations for Treatment Choices
- How Long Does It Take for Paxil to Work?
- Factors Influencing Onset of Action
- Patient Insights
- Tips for Managing Panic Disorder Alongside Paxil Treatment
- Utilize Mindfulness Techniques
- Build a Support Network
Paxil and Panic Disorder
Paxil, or paroxetine, plays a significant role in managing panic disorder. This medication belongs to a class known as selective serotonin reuptake inhibitors (SSRIs), which work by increasing serotonin levels in the brain.
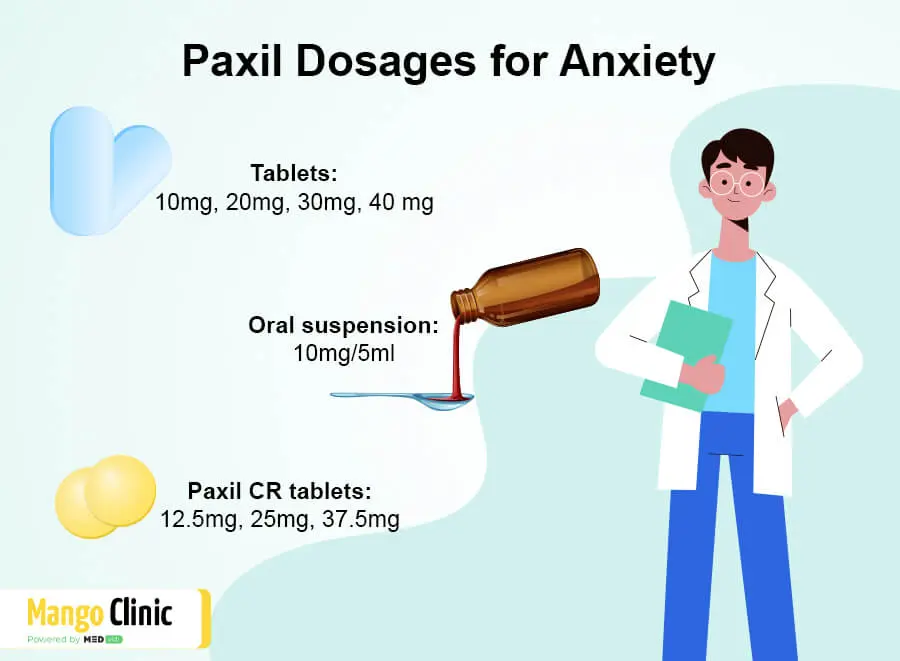
Dosage typically begins at a low level, often around 10 mg per day, to minimize side effects. Adjustments can occur based on individual responses, with common dosages ranging from 20 mg to 60 mg daily.
Regular monitoring is beneficial during treatment. Patients should maintain open communication with their healthcare provider regarding any side effects or concerns. Common side effects may include:
- Nausea
- Sleep disturbances
- Dry mouth
- Fatigue
Improvements in anxiety and panic symptoms can take several weeks. For maximum effectiveness, adhering to the prescribed regimen is key.
Combination therapy with cognitive-behavioral therapy (CBT) often enhances treatment outcomes. CBT helps patients develop coping strategies and address the triggers of panic attacks.
Paxil may not be suitable for everyone. Individuals with certain medical conditions, such as liver disease or seizures, should discuss their options with a healthcare provider. Pregnant or breastfeeding individuals also require careful consideration of risks and benefits.
Withdrawal symptoms can occur if Paxil is discontinued abruptly. Tapering off the medication under medical supervision is advisable to mitigate these effects.
In summary, Paxil acts effectively against panic disorder when used correctly. Regular follow-ups and open dialogue with healthcare providers remain crucial for a successful treatment plan.
Understanding Panic Disorder Symptoms
Panic disorder manifests through intense physical and psychological symptoms that can occur unexpectedly. Recognizing these signs is crucial for timely intervention. Common symptoms include rapid heartbeat, shortness of breath, dizziness, and a feeling of impending doom. Individuals might also experience sweating, trembling, and chest pain, which can often mimic a heart attack.
Physical Symptoms
Physical reactions during a panic attack are intense. Heart palpitations can make you feel as though your heart is racing out of control. Shortness of breath may lead to feelings of choking, while chest discomfort could trigger anxiety about heart health. Sometimes, individuals report nausea or gastrointestinal issues which complicate the emotional experience.
Psychological Symptoms
The psychological aspect is equally challenging. Many report feelings of depersonalization or detachment from reality. This disconnection can heighten feelings of anxiety and fear, leading to avoidance behaviors. Anticipating future panic attacks may also result in significant lifestyle changes, such as avoiding certain places or situations where attacks have occurred.
Seek professional help if these symptoms impact your daily life. Early recognition and treatment can substantially improve quality of life. Identifying triggers and managing stress through therapy, medication, or lifestyle changes can provide relief and promote well-being.
The Role of Paxil in Treating Panic Disorder
Paxil, a selective serotonin reuptake inhibitor (SSRI), stands out as a reliable option for managing panic disorder. By increasing serotonin levels in the brain, it helps alleviate the frequency and intensity of panic attacks.
Key benefits of Paxil include:
- Reduction in the occurrence of panic attacks.
- Improvement in overall anxiety levels.
- Enhanced quality of life and daily functioning.
Studies show that Paxil is effective for a majority of patients, with noticeable improvements often observed within a few weeks of starting treatment. It’s essential to follow the prescribed dosage and schedule for optimal results. Healthcare providers typically recommend a gradual increase in dosage to minimize side effects.
Some common side effects may include:
- Nausea
- Fatigue
- Headaches
- Weight gain
These side effects usually diminish over time. It’s crucial to communicate any concerns with a healthcare professional to adjust treatment if needed.
Combining Paxil with cognitive-behavioral therapy (CBT) often enhances its effectiveness. CBT equips patients with practical tools to manage anxiety, making the recovery journey smoother.
Regular follow-ups allow for adjustments to the treatment plan as necessary. Always consult a doctor before discontinuing Paxil, as sudden withdrawal may lead to withdrawal symptoms.
In summary, Paxil plays a significant role in treating panic disorder. Its established efficacy, combined with psychotherapy, offers a pathway to improved mental health. Engage openly with healthcare providers to find the best approach for individual needs.
Dosage Guidelines for Paxil in Panic Disorder
The recommended starting dose of Paxil (paroxetine) for treating panic disorder is 10 mg per day. This dosage allows the body to adjust to the medication while minimizing side effects.
If patients tolerate the initial dose well, it can be increased to 20 mg after one week. Further adjustments can be made based on individual response and tolerability, with a maximum recommended dose of 60 mg per day. Regular follow-ups with a healthcare provider are crucial to determine the most effective dosage.
Gradual dosing is important to mitigate potential withdrawal effects and to monitor for any adverse reactions. Patients should communicate any side effects to their healthcare provider promptly.
| Dosage Level | Duration |
|---|---|
| 10 mg | Starting dose |
| 20 mg | After 1 week if tolerated |
| 60 mg | Maximum daily dose |
Adjustments should be made thoughtfully, as some individuals may respond better to lower doses. Regular monitoring by a healthcare provider helps ensure optimal treatment outcomes while maintaining safety.
Potential Side Effects of Paxil
Paxil may lead to side effects that require attention. Common reactions include nausea, fatigue, and dizziness. Some individuals may also experience dry mouth or changes in appetite, prompting monitoring of food intake and hydration levels.
Emotional shifts can arise, including increased anxiety or mood swings. It’s vital to communicate any significant changes to a healthcare provider promptly for appropriate adjustments in treatment.
Paxil may impact sexual function, causing difficulties such as decreased libido or issues achieving orgasm. Open discussions with healthcare professionals can help in managing these symptoms, potentially through adjusting dosage or considering alternative medications.
Allergic reactions, while less common, can occur. Signs to watch for include rash, itching, or swelling. If these symptoms appear, seeking medical assistance is essential.
In rare cases, Paxil may contribute to serotonin syndrome, a serious condition characterized by confusion, rapid heart rate, or increased blood pressure. Recognizing these symptoms early is critical, and immediate medical attention is necessary.
Withdrawal symptoms can manifest if Paxil is abruptly stopped. Gradual discontinuation under a doctor’s guidance is recommended to minimize potential discomfort.
Staying informed about side effects and maintaining open communication with healthcare providers ensures safe and effective management of treatment with Paxil.
Comparing Paxil to Other Treatments for Panic Disorder
Paxil (paroxetine) is a selective serotonin reuptake inhibitor (SSRI) commonly prescribed for panic disorder. Clinical studies show that Paxil can significantly reduce the frequency and intensity of panic attacks in many patients. The usual effective dose ranges from 10 mg to 60 mg daily, depending on individual tolerance and response.
While Paxil is effective, several alternative treatments also exist. Cognitive Behavioral Therapy (CBT) stands out as a primary non-pharmacological method. CBT focuses on addressing the thought patterns that contribute to panic attacks, equipping patients with coping strategies. Research indicates that CBT often yields lasting results, sometimes even after treatment ends.
Comparative Effectiveness of SSRIs and Benzodiazepines
Other SSRIs, like Prozac (fluoxetine) and Zoloft (sertraline), share similar benefits with Paxil in treating panic disorder. These medications also work by increasing serotonin levels but may have different side effect profiles that could influence the choice of treatment. Patients should consult with their healthcare provider about which SSRI may be more suitable for their specific case.
Benzodiazepines, such as Lorazepam and Alprazolam, offer rapid relief from panic attacks. While effective for immediate anxiety management, they carry a risk of dependence and are generally recommended for short-term use only. This makes SSRIs like Paxil preferable for long-term treatment strategies.
Considerations for Treatment Choices
Choosing between Paxil and other options depends on individual needs, potential side effects, and the nature of the panic disorder. Monitoring by a healthcare professional is essential throughout treatment to ensure optimal outcomes and to adjust strategies as necessary. This personalized approach can make a significant difference in a patient’s recovery journey.
How Long Does It Take for Paxil to Work?
Paxil typically begins to show effects on anxiety and panic disorder within 4 to 6 weeks of consistent use. However, some individuals may notice improvements in symptoms as early as 1 to 2 weeks into treatment. These early benefits can include reduced anxiety and a greater sense of well-being.
Factors Influencing Onset of Action
Patient Insights
Many patients report that the key to seeing results is maintaining a consistent medication schedule. Taking Paxil at the same time each day can help stabilize blood levels of the medication, leading to more predictable effects. While patience is crucial, staying engaged with your treatment process through regular check-ins with your healthcare provider can enhance the overall effectiveness of Paxil for managing panic disorder.
Tips for Managing Panic Disorder Alongside Paxil Treatment
Incorporate regular physical activity into your routine. Aim for at least 30 minutes of exercise most days. Activities like walking, jogging, or yoga can significantly reduce anxiety and improve mood.
Practice deep breathing exercises. Spend a few minutes each day focusing on your breath. Inhale slowly through your nose, hold for a few seconds, and exhale through your mouth. This technique can help calm your nervous system when panic symptoms arise.
Utilize Mindfulness Techniques
Engage in mindfulness or meditation practices. Set aside time each day to focus on the present moment. Use apps or guided sessions to help you stay grounded and reduce anxiety levels.
Establish a consistent sleep schedule. Aim for 7-9 hours of sleep each night. Good sleep hygiene supports emotional regulation and broadens your ability to cope with stress.
Build a Support Network
Connect with friends or family who understand your situation. Share your experiences and lean on them for support. Joining a support group can also provide an opportunity to gain insights and coping strategies from others facing similar challenges.
Communicate openly with your healthcare provider. Discuss your treatment progress, side effects, and any new strategies you want to try. Regular check-ins help you stay informed and make necessary adjustments to your treatment plan.