Plavix is often prescribed for those at risk of heart attack or stroke due to its ability to prevent blood clots. If your doctor recommends it, ensure you understand the dosage and adherence to the prescribed schedule. Typically, a daily dose of 75 mg is standard, but your healthcare provider may adjust it based on your condition.
This medication works by inhibiting platelets from aggregating, significantly lowering the chance of clot formation. Monitor your response to the drug regularly, particularly for any signs of unusual bleeding or bruising, as these can indicate serious side effects. Always communicate any concerns with your healthcare provider to ensure optimal management of your treatment.
Combining Plavix with certain medications or supplements can alter its effectiveness. Be proactive in discussing all other drugs and health products you are using. Additionally, lifestyle modifications, such as quitting smoking and adopting a heart-healthy diet, can enhance the benefits of Plavix.
- Detailed Overview of Plavix Prescription Drug
- Dosage and Administration
- Side Effects and Precautions
- Mechanism of Action of Plavix
- Inhibition of ADP Receptors
- Impact on Cardiovascular Events
- Indications for Plavix Prescription
- Post-Myocardial Infarction
- Cerebrovascular Disease
- Dosage Guidelines for Plavix Use
- Potential Side Effects and Risks of Plavix
- Interactions with Other Medications
- Common Drug Interactions
- Inhibitors and Inducers
Detailed Overview of Plavix Prescription Drug
Plavix, generically known as clopidogrel, plays a pivotal role in reducing the risk of heart attacks and strokes in individuals with cardiovascular conditions. This antiplatelet medication inhibits platelet aggregation, effectively preventing clot formation. Healthcare providers commonly prescribe Plavix following procedures like stent placement or heart bypass surgery.
Dosage and Administration
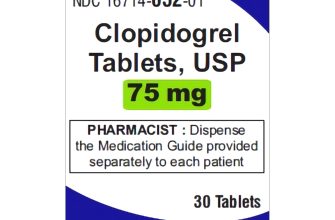
The standard dosage for Plavix is typically 75 mg once daily, though some patients may receive a loading dose of 300 mg. Patients should swallow the tablet whole without crushing or splitting, ensuring optimal absorption. It’s crucial to take Plavix consistently at the same time every day to maintain stable drug levels in the bloodstream.
Side Effects and Precautions
Common side effects of Plavix include bruising, bleeding, and gastrointestinal discomfort. Some individuals may experience more severe reactions like allergic responses or severe bleeding. Those with a history of gastrointestinal bleeding, liver disease, or certain allergies should discuss their medical history with their healthcare provider before starting this medication. Regular monitoring is advised to identify potential complications early.
Always inform healthcare professionals about other medications being taken, as some can interact with Plavix, reducing its effectiveness or increasing the risk of bleeding. For instance, combining Plavix with non-steroidal anti-inflammatory drugs (NSAIDs) or other anticoagulants may heighten bleeding risks, necessitating careful evaluation of treatment plans.
Consult your doctor regularly to adjust dosages or explore alternative treatments if needed. Prioritize clear communication regarding any unusual symptoms or concerns while on Plavix to ensure personalized and safe healthcare management.
Mechanism of Action of Plavix
Plavix, or clopidogrel, operates primarily as an antiplatelet medication. It inhibits platelet aggregation, which is critical in preventing blood clots. After oral administration, Plavix is metabolized in the liver to produce an active metabolite. This metabolite irreversibly binds to the P2Y12 receptors on the surface of platelets.
Inhibition of ADP Receptors
The P2Y12 receptor is part of the ADP receptor family. When activated by adenosine diphosphate (ADP), these receptors promote platelet activation and aggregation. By blocking these receptors, Plavix effectively prevents platelet activation, reducing the risk of thrombus formation. This action is essential for patients with cardiovascular diseases, particularly those who have experienced myocardial infarctions or strokes.
Impact on Cardiovascular Events
Utilizing Plavix helps lower the incidence of major cardiovascular events. It is commonly prescribed alongside aspirin for maximum benefit, known as dual antiplatelet therapy (DAPT). This combination significantly enhances protective effects against future cardiac events, making it a key part of treatment protocols in high-risk patients.
Indications for Plavix Prescription
Plavix is primarily prescribed to reduce the risk of heart attack and stroke in patients with a history of cardiovascular disease. It works by preventing blood clots, making it a key player in managing various conditions related to the heart and blood vessels.
Post-Myocardial Infarction
Patients who have experienced a myocardial infarction (heart attack) are often prescribed Plavix to prevent further incidents. This medication helps maintain blood flow by inhibiting platelet aggregation, which minimizes the chance of subsequent clots.
Cerebrovascular Disease
For individuals with a history of stroke or transient ischemic attacks (TIA), Plavix serves as a preventive measure. By reducing platelet clumping, it lowers the likelihood of another stroke or TIA occurring. Patients with peripheral arterial disease may also benefit from its use to promote better circulation.
Additionally, Plavix is recommended for patients undergoing certain types of heart procedures, such as stent placement, to reduce the risk of restenosis and improve long-term outcomes. Always consult a healthcare professional to determine the most appropriate treatment plan tailored to individual health needs.
Dosage Guidelines for Plavix Use
Begin with a standard dosage of 75 mg once daily. This dosage is typically sufficient for most patients after a loading dose.
A loading dose of 300 mg may be given for patients who require rapid antiplatelet efficacy, but this is often reserved for those undergoing certain procedures or at high risk for cardiovascular events.
The following considerations apply to Plavix dosing:
- Weight-Based Adjustments: Individuals weighing less than 60 kg may benefit from tailoring the dosage; consult a healthcare provider for specific instructions.
- Age Factors: Elderly patients may require monitoring due to potential increased sensitivity. Adjustments based on renal function may also be necessary.
- Drug Interactions: Co-administration with certain medications, particularly those affecting CYP2C19 metabolism, warrants careful evaluation of Plavix dosage. Medications such as omeprazole may reduce efficacy.
- Post-Myocardial Infarction: In patients post-MI, the standard dosage remains at 75 mg daily, often in conjunction with aspirin therapy.
Monitor for signs of bleeding or bruising, which may indicate the need for dosage adjustments. Regular follow-up with a healthcare provider is recommended to ensure optimal therapy.
Always consult with a physician before making any changes to medication regimens. Each patient’s condition and response to treatment may vary significantly.
Potential Side Effects and Risks of Plavix
Patients using Plavix should be aware of potential side effects and risks associated with this medication. Monitoring for any adverse reactions is essential.
The most common side effects include:
| Side Effect | Frequency |
|---|---|
| Bleeding complications | Common |
| Nausea | Occasional |
| Diarrhea | Occasional |
| Rash | Uncommon |
| Headache | Uncommon |
Bleeding risks, particularly gastrointestinal bleeding, are significant. Report any unusual bleeding, such as in urine or stool, immediately to your healthcare provider. Regular blood tests may be necessary to monitor platelet levels.
Allergic reactions can occur, presenting as swelling, itching, or difficulty breathing. Seek urgent medical attention if these symptoms arise.
Interactions with other medications can heighten risks. Inform your doctor about all medications you are currently taking to avoid dangerous combinations.
Special considerations apply to patients with liver disease, as Plavix metabolism can be affected, increasing the likelihood of side effects. Discuss personal medical history with your physician to ensure safe use.
In summary, while Plavix serves as an important antiplatelet agent, awareness and communication about potential side effects remain critical for safe treatment outcomes.
Interactions with Other Medications
Plavix may interact with several medications, impacting its effectiveness. Always disclose your current medications to your healthcare provider before starting Plavix.
Common Drug Interactions
Taking Plavix alongside certain medications can increase the risk of bleeding. Nonsteroidal anti-inflammatory drugs (NSAIDs) like ibuprofen and naproxen, as well as anticoagulants such as warfarin, should be used cautiously, as they can enhance blood-thinning effects.
Some antidepressants, including selective serotonin reuptake inhibitors (SSRIs), may also pose a risk. Consult your doctor to determine suitable alternatives if you require these medications.
Inhibitors and Inducers
Drugs that inhibit the enzyme CYP2C19, such as omeprazole and esomeprazole, can reduce Plavix’s effectiveness. Discuss your treatment options with your healthcare provider to avoid these inhibitors if you’ve been prescribed Plavix.
Conversely, certain medications may induce CYP2C19 activity and might affect Plavix’s metabolism. Always communicate any changes in your medication regimen with your healthcare provider to ensure safety and effectiveness in your treatment plan.